Mr Lower is an experienced gynaecologist who is able to offer advice on a wide range of gynaecological conditions. He receives many referrals from other gynaecologists for conditions where he is known to have particular expertise and he is always ready to refer his patients to colleagues for expert treatment of conditions with which he is less familiar.
The areas where he is known to have particular expertise include:
Asherman’s Syndrome
Asherman’s syndrome is a condition where adhesions form inside the uterus causing the front and back walls to stick together. It usually follows a D&C performed after a miscarriage, termination of pregnancy, or following a retained placenta. The condition is usually much worse if there has been infection at the same time. It can also occur after surgery such as a myomectomy, Caesarean section, or a foreign body such as an IUCD.
Symptoms
Asherman’s syndrome usually causes a reduction or complete cessation of the menstrual flow and is often associated with pain. It is also cause infertility and recurrent miscarriage.
Diagnosis and treatment
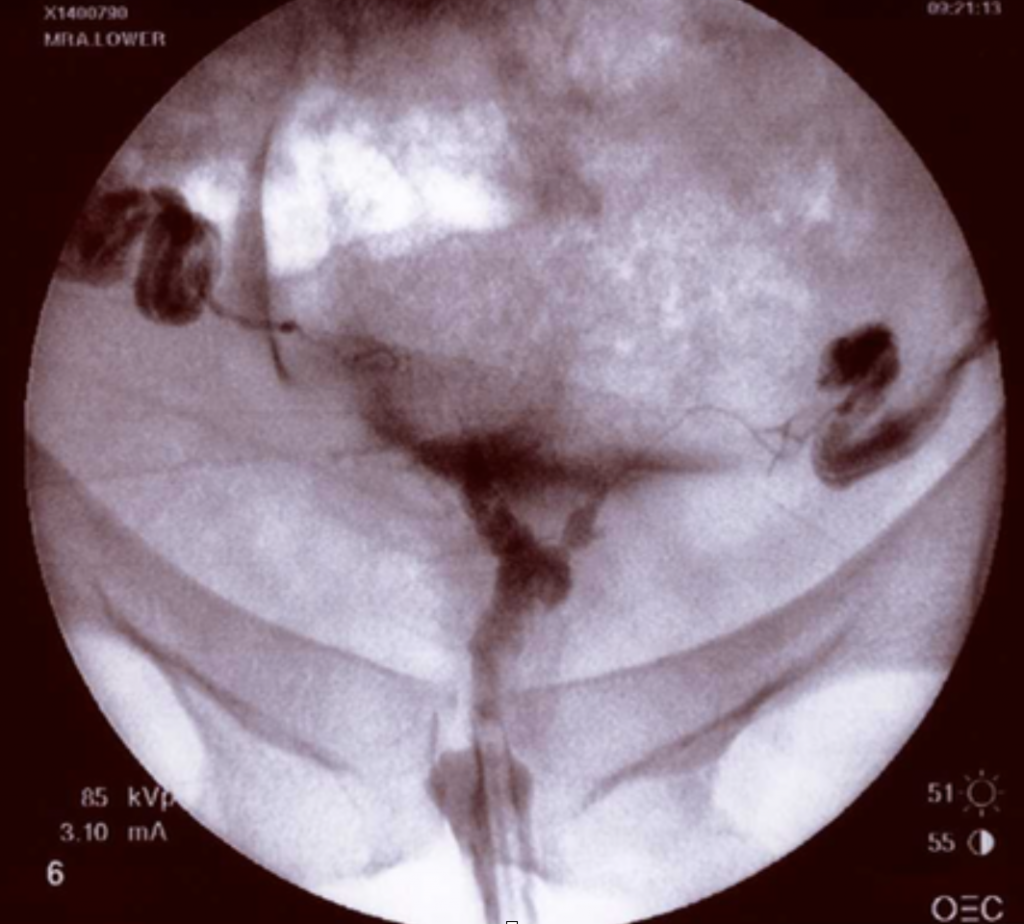
Asherman’s syndrome can be diagnosed by hysterosalpingogram, saline sonography or hysteroscopy. 3D ultrasound is also useful in assessing the endometrium. Treatment is by hysteroscopic division of the adhesions at the time of the initial hysteroscopy. In more severe cases we will usually insert a stent combined with high-dose oestrogen therapy for one or two months following surgery. The stent is usually removed after a month or so and this will divide any small adhesions which may have reformed.
The image below is a hysterosalpingogram which shows the presence of an isolated adhesion within the uterus.
For more information about Asherman’s Syndrome folllow this link to the Asherman’s Surgical Centre website
Uterine Fibroids
Fibroids are benign (non-cancerous) tumours or growths affecting the uterus. The uterus is composed almost entirely of muscle fibres which are not capable of voluntary contraction but nonetheless contract strongly during childbirth, expelling the baby through the birth canal.
Fibroids are not composed of fibrous tissue at all, but each fibroid appears to grow by clonal replication of a single muscle cell. In other words, a single muscle cell starts to grow and replicate itself many thousands of times over, creating a firm muscular tumour with some associated new blood vessels and supporting tissues within it.
The normal controlling mechanisms restricting growth and replication of individual cells appear to be lost when a fibroid starts to grow. It is not clear why this happens, nor why some fibroids grow more rapidly than others and why some women have a greater tendency to develop fibroids than others.
Diagnosis
This is usually made by ultrasound scan or MRI. The latter is better for distinguishing adenomyosis.
Treatment
Usually, surgery is the best option, where possible Mr Lower will offer laparoscopic myomectomy or keyhole surgery. For very large fibroids open myomectomy is better, and for complex situations, uterine artery embolisation has a part to play.
Uterine Abnormalities (Septum and isthmocele)
Uterine abnormalities can be caused by abnormal development in the uterus (congenital) or as a result of injury in later life (acquired).
The uterus is formed as a result of the fusion of two embryonic tubular structures called Mullerian ducts. Incomplete fusion of these ducts as the embryo develops causes a partial or full separation of the uterus resulting in a range of abnormalities termed Mullerian Duct abnormalities, ranging from a partial or full uterine septum to two completely separate uterine bodies and cervices (Uterus didelphys).
Surgical correction of some of these such as uterine septum can be accomplished by complex hysteroscopic surgery. Mr Lower is expert in assessing and treating such conditions.
Sometimes abnormalities of the uterus can result from the incomplete healing of surgical scars from procedures such as Caesarean section. The resulting defect in the Caesarean section scar in the wall of the uterus is termed a uterine diverticulum or an isthmocele. Mr Lower is one of a very few surgeons in the UK with experience in treating such defects by laparoscopic excision and repair.
Ovarian cysts
Each month the ovary will develop a follicle which usually grows to around 2 cm in diameter before it ruptures, releasing a healthy egg which can then be fertilised. The ovary is also susceptible to pathological cysts, the most common of which are endometriotic cysts, also known as chocolate cysts. There are a number of other causes of benign cysts, including cyst adenoma, dermoid cysts and fibromas. They all have characteristic ultrasound appearances and can usually be readily distinguished from malignant cysts which are much less common, especially amongst younger women, but it is important to exclude the possiblity of malignancy and the best way to do this is to remove the cyst, with conservation of the normal portion of the ovary if possible and appropriate. An ovarian cyst may also cause the ovary to become slightly unstable, making the chance of torsion about its vascular pedicle more likely. This can result in emergency admission with acute pelvic pain and if not operated on at this point to reduce the torsion can lead to loss of the ovary.
Treatment
Lapaoroscopic ovarian cystectomy is the treatment of choice for ovarian cysts and quite large cysts up to 20cm in diameter can be dealt with providing the correct techniques are employed. Mr Lower is an expert in this type of surgery and it is usually accomplished as a day case with rapid return to work within a few days.
Pelvic Adhesions
Mr Lower is an expert in the treatment and prevention of pelvic adhesions. Adhesions result from previous surgery or infection. They are an exagerated respoinse to the healing process and form a film-like wrapping of the pelvic organs, often resembling cling film, which can become fibrous and dense as they mature. Adhesions cause pain and can restrict the mobility of the Fallopian tubes, partially or fully blocking them leading to infertility.
Early pregnancy complications
Ectopic pregnancy
Fertilisation of the egg by the sperm usually occurs in the Fallopian tube and the fertilised egg, or embryo as it is called at this time, will travel down the Fallopian tube to the uterus where it will implant. Sometimes the embryo fails to travel down the Fallopian tube and will try to implant in the Fallopian tube resulting in an ectopic pregnancy. This is more common if the Fallopian tube has been damaged by prior infection (especially chlamydia) or surgery to the Fallopian tube or a previous ectopic pregnancy. Many ectopic pregnancies will miscarry but some will go on to develop and gain a sizeable blood supply and the thin wall of the tube ruptures at between 6 and 8 weeks of gestation leading to severe abdominal pain and often catastrophic haemorrhage into the peritoneal cavity. This condition is very definitely a medical emergency requiring urgent surgery and often results in removal of the Fallopian tube to control the bleeding.
Ectopic pregnancies can often be picked up prior to rupture by early ultrasound scanning and semi-elective surgery can be offered when the Fallopian tube can sometimes be saved and just the pregnancy tissue is removed. An alternative can be to use medical treatment with methotrexate to induce a miscarriage of the ectopic pregnancy. In either case careful follow-up checking serial hCG hormone estimation is required to ensure that the condition is resolving satisfactorily.
Miscarriage
Miscarriage is a very common, multifactorial complication of early pregnancy. One in four pregnancies may miscarry and the most common cause is chromosomal abnormality which cannot be treated after conception. There are a number of conditions which are potentially treatable, and after 2 or 3 miscarriages it is worth undergoing investigations to see whether treatment can reduce the risk of a further miscarriage.
If no other cause is identified, IVF with PGT-A (pre-implantation testing for aneuploidy or abnormal numbers of chromosomes) can identify normal embryos that are less likely to miscarry. However this relies one good ovarian reserve.
In such cases it is also mandatory to check both potential parents chromosomes to check whether they carry a balanced abnormality of their chromosomes.
Endometriosis
Endometriosis is a condition in which the tissue that lines the uterus, the endometrium, develops in abnormal sites, typicaly on the bowel, the outside of the uterus, the ovaries and the peritoneum. Rarely it can also develop in the lungs and pleura surrounding the lungs.
Like the endometrium, endometriosis tissue undergoes cyclical changes in response to the natural hormonal cycles, leading to loss of the glandular tissue and bleeding like menstruation from the sites of endometriosis implants. This causes fibrosis and scarring leading to cyclical pain at the sites of the implants, heavy and painful periods and pain with sex (dyspareunia). On average it takes 8 years to establish a definitive diagnosis of endometriosis in the UK. In some parts of the world it can take as long as 10 years. Mr Lower has recently started using the novel Endosure test as a non-invasive means of establishing an early diagnosis. The Endosure test measures the myoelectrical activity of the intestines, which is altered in women with endometriosis. Further information about Endosure is available here.
The curious thing about endometriosis is that the symptoms it causes are not related to the size or extent of the lesions. Therefore some women can experience disabling pain with only a small isolated spot of endometriosis which may not cause any symptoms in another woman, whilst others can have very extensive endometriosis with adhesions and scarring affecting the bowel, ovaries and peritoneum and yet have very little in the way of symptoms.
For those who are affected, the symptoms can be controlled to some extent with hormones and are often relieved by pregnancy, but endometriosis can cause delay in conception and the condition is found in up to 30% of women presenting with infertility.
Treatment
Medical treatment incudes the use of progesterone, either orally or from the Mirena intrauterine system, oral contraceptives, gonadotrophin releasing hormone analogues (GnRH-a) such as Zoladex which is given by monthly injection and causes temporary reduction of oestrogen levels and menopausal symptoms which also causes temporary shrinkage of the endometriosis lesions.
Surgery to ablate or excise the areas of endometriosis is very successfuland has been shown to improve the chance of spontaneous conception. Up to 80% of women will remain asymptomatic for up to 5 years following such surgery and many will conceive during this window, not least because sex can be less painful. Laparoscopy with laser ablation is Mr Lower’s treatment of choice for this condition, endometriotic cysts can also be treated in this way, but sometimes the disease is so extensive that a more difficult and demanding operation is required, with removal of affected segments of bowel in the worst cases